Uterine fibroids
 |
| Uterine fibroids |
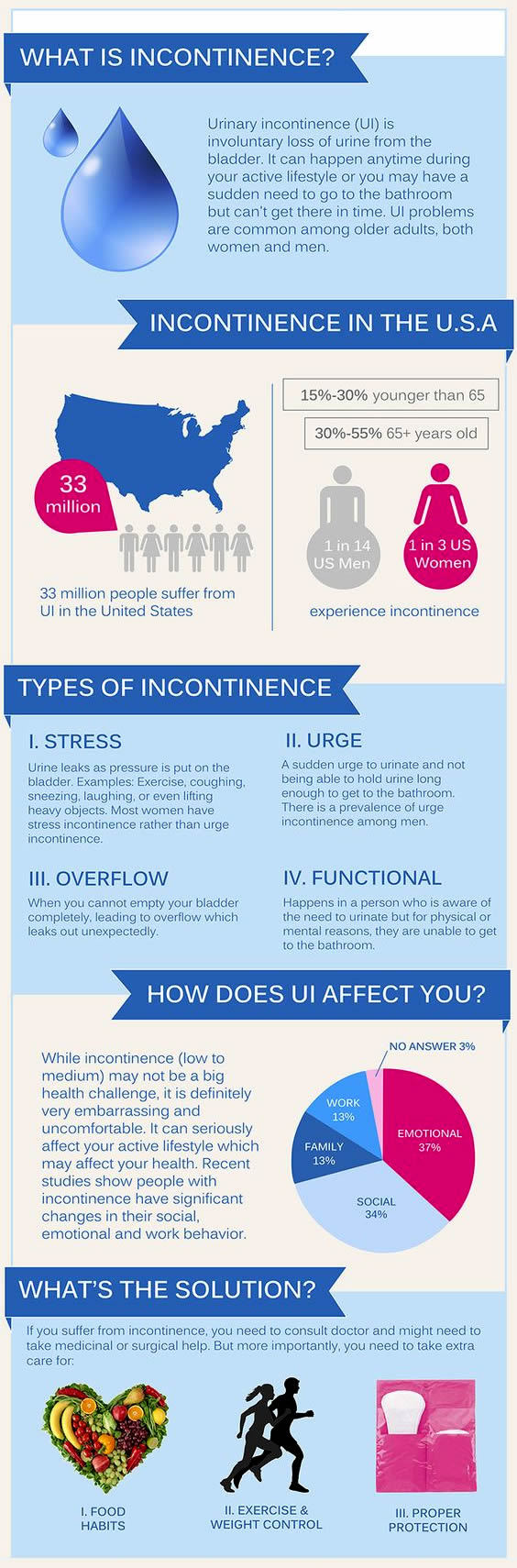
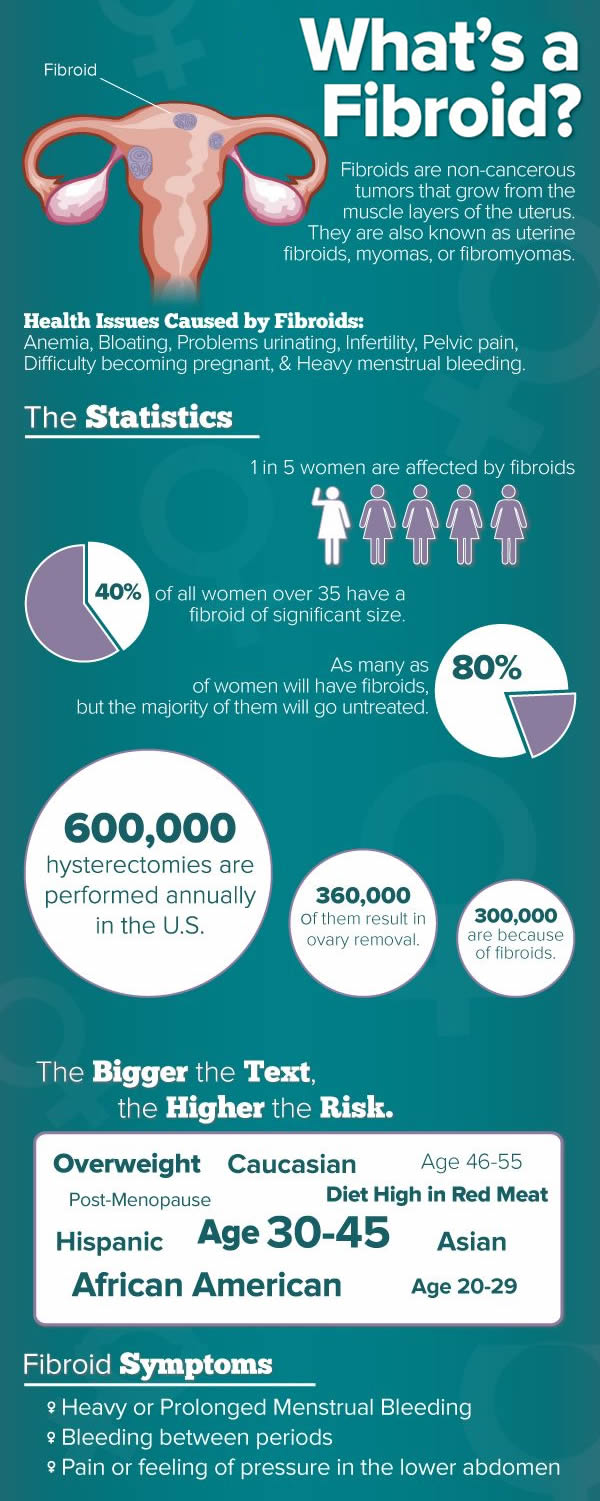
Uterine fibroids (also called leiomyomas or myomas) are benign growths of the muscle inside the uterus. They are not cancerous, nor are they related to cancer. Fibroids can cause a wide variety of symptoms, including heavy menstrual bleeding and pressure on the pelvis.
Description
Uterine fibroids are extremely common. About 25% of women in their reproductive years have noticeable fibroids. There are probably many more women who have tiny fibroids that are undetected.
Fibroids develop in women between the ages of 30–50. They are never seen in women younger than 20 years old. After menopause, if a woman does not take estrogen, fibroids shrink. It appears that African American women are much more likely to develop uterine fibroids.
  |
Fibroids are divided into different types, depending on the location. Submucous fibroids are found in the uterine cavity; intramural fibroids grow on the wall of the uterus; and subserous fibroids are located on the outside of the uterus. Many fibroids are so large that they fit into more than one category. The symptoms caused by fibroids are often related to their location.
Causes and symptoms
No one knows exactly what causes fibroids. The growth of fibroids, however, appears to depend on the hormone estrogen. Fibroids often grow larger when estrogen levels are high, as in pregnancy. Medications that lower the estrogen level can cause the fibroids to shrink.
The signs and symptoms of fibroids include:
- Heavy uterine bleeding. This is the most common symptom, occurring in 30% of women who have fibroids. The excess bleeding usually happens during the menstrual period. Flow may be heavier, and periods may last longer. Women who have submucous or intramural fibroids are most likely to have heavy uterine bleeding.
- Pelvic pressure and pain. Large fibroids that press on nearby structures such as the bladder and bowel can cause pressure and pain. Larger fibroids tend to cause more severe symptoms.
- Infertility. This is a rare symptom of fibroids. It probably accounts for less than 3% of infertility cases. Fibroids can cause infertility by compressing the uterine cavity. Submucous fibroids can fill the uterine cavity and interfere with implantation of the fertilized egg.
- Miscarriage. This is also an unusual symptom of fibroids, probably accounting for only a tiny fraction of the miscarriages that occur.
- Pregnancy complications. Fibroids can greatly increase in size during pregnancy, because of increased levels of estrogen. They can cause pain, and even lead to premature labor.
Diagnosis
A healthcare provider can usually feel fibroids during a routine pelvic examination. Ultrasound can be used to confirm the diagnosis, but this is not generally necessary.
Treatment
There are several natural treatments that help lower estrogen levels and slow the growth of the benign tumors. One study of alternative and complementary treatments for uterine fibroids found, however, that the cost of the alternative remedies was significantly higher than the cost of conventional treatments.
Nutritional therapy
There are several things women can do nutritional-wise to avoid having fibroids or prevent them from getting bigger:
- Eat more fruits, green or sea vegetables, whole grains, nuts, and seeds.
- Eat more soy foods such as tofu, tempeh, miso, or soy burger. Soy products contain isoflavones, which help reduce high levels of estrogens in the body.
- Avoid foods with high fat or sugar content, caffeine,or alcohol.
- Avoid eating produce sprayed with insecticides.
Nutritional supplements
The following supplements may be helpful in lowering estrogen levels and controlling fibroids:
- Bromelain: reduces inflammation.
- Choline: may improve liver function.
- Flaxseed: helps reduce excessive production of estrogens and other hormones.
- Vitamin E and evening primrose oil: help to regulate hormone production and may even shrink the fibroids.
- Vitamin C and bioflavonoids: have antiinflammatory and antioxidant effects.
Herbal treatment
Kuei-chih-fu-ling-wan (Keishi-bukuryo-gan; KBG) is a traditional Chinese herbal preparation that can effectively shrink fibroid tumors in 60% of patients, according to one study conducted by Japanese scientists. KBG is a mixture of the following herbs: cassia bark (Keihi), herbaceous peony roots (Shakuyaku), peach kernels (Tounin), herbaceous fungus (Bukuryo), and root bark of peony (Botanpi).
In addition to reducing fibroid size, KBG also successfully alleviated fibroid symptoms such as severe menstrual bleedings or menstrual pain in 90% of the women in the study. These researchers suggest that KBG may work by inhibiting the production of sex hormones including estrogen.
Unlike many other presently available herbal preparations that may be effective but lack scientific evidence to support their uses, KBG is proven safe as well as having few side effects. Women with fibroids, therefore, have one more alternative treatment to hysterectomy.
There are many herbal formulas that can be used depending on specific symptoms and body types. Another herbal treatment that may also be effective is wild yam progesterone cream. However, these are potent drugs and patients should consult their doctors before trying any of these treatments.
Homeopathy
A homeopathic physician may prescribe patient-specific homeopathic remedies to control fibroid symptoms.
Allopathic treatment
Not all fibroids cause symptoms. Even fibroids that do cause symptoms may not require treatment. In the majority of cases, the symptoms are inconvenient and unpleasant, but do not result in health problems.
Occasionally, fibroids lead to such heavy menstrual bleeding that the woman becomes severely anemic. In these cases, treatment of the fibroids may be necessary. Very large fibroids are much harder to treat. Therefore, many doctors recommend treatment for moderatelysized fibroids, in order to prevent them from growing into large fibroids that cause worse symptoms.
The following are possible treatment plans:
- Observation (watchful waiting). Most women already have symptoms at the time their fibroids are discovered, but feel that they can tolerate their symptoms. Therefore, no active treatment is given, but the woman and her physician stay alert for signs that the condition might be getting worse.
- Hysterectomy. This procedure involves surgical removal of the uterus, and it is the only definitive cure for fibroids. In fact, 25% of hysterectomies are performed because of symptomatic fibroids. A gynecologist can remove a fibroid uterus during either an abdominal or a vaginal hysterectomy. The choice depends on the size of the fibroids and other factors such as previous births and previous surgeries.
- Myomectomy. In this surgical procedure only the fibroids are removed; the uterus is repaired and left in place. This is the surgical procedure many women choose if they are not finished with childbearing. At first glance, it seems that this treatment is a middle ground between observation and hysterectomy. However, myomectomy is actually a difficult surgical procedure, more difficult than a hysterectomy. Myomectomy often causes significant blood loss, and blood transfusions may be required. In addition, some fibroids are so large, or buried so deeply within the wall of the uterus, that it is not possible to save the uterus, and a hysterectomy must be done, even though it was not planned.
- Lowering estrogen levels. Since fibroids are dependent on estrogen for their growth, medical treatments that lower estrogen levels can cause fibroids to shrink. A group of medications known as GnRH antagonists can dramatically lower estrogen levels. Women who take these medications for three to six months find that their fibroids shrink in size by 50% or more. They usually experience dramatic relief of their symptoms of heavy bleeding and pelvic pain.
- Uterine artery embolization (UAE). Embolization is a newer alternative to hysterectomy that shrinks fibroids by cutting off their blood supply. In UAE, the surgeon inserts a catheter into the uterine arteries. Small particles of polyvinyl foam or other inert substances are injected through the catheter into the arteries. The particles form an embolus, or clump, that blocks the blood supply to the fibroids and causes them to shrink. UAE is still controversial, however, because it has been associated with significant complications.
Unfortunately, GnRH antagonists cause unpleasant side effects in over 90% of women. The therapy is usually used for only three months, and should not be used for more than six months because the risk of developing brittle bones (osteoporosis) begins to rise.
Once the treatment is stopped, the fibroids begin to grow back to their original size. Within six months, most of the old symptoms return. Therefore, GnRH agonists cannot be used as long-term solution.
 |
| Uterine fibroids infographic |
At the moment, treatment with GnRH antagonists is used mainly in preparation for surgery (myomectomy or hysterectomy). Shrinking the size of the fibroids makes surgery much easier, and reducing the heavy bleeding allows a woman to build up her blood count before surgery.
Fibroids can cause problems during pregnancy because they often grow in size. Large fibroids can cause pain and lead to premature labor.
Fibroids cannot be removed during pregnancy because of the risk of injury to the uterus and hemorrhage. GnRH antagonists cannot be used during pregnancy. Treatment is limited to pain medication and medication to prevent premature labor, if necessary.
Expected results
Many women who have fibroids have no symptoms or have only minor symptoms of heavy menstrual bleeding or pelvic pressure. However, fibroids tend to grow over time, and gradually cause more symptoms. Many women ultimately decide to have some form of treatment. Currently, hysterectomy is the most popular form of treatment.
Prevention
Eating a healthful diet, reducing stress, and exercising regularly is the preferred preventive treatment regimen of many diseases including fibroids.