Vomiting
 |
| Vomiting |
Vomiting is the forceful discharge of stomach contents through the mouth.
Vomiting, also called emesis, is a symptomatic response to any number of harmful triggers. Vomiting is a forceful expulsion, and is different from regurgitation — the effortless return of stomach contents to the mouth. Although unpleasant, vomiting is an important function because it rids the body of harmful substances.
Vomiting is a complex process resulting from the coordinated interaction of nerve pathways, the brain, and muscles of the gastrointestinal system
  |
This structure is exposed to chemicals in the bloodstream and the cerebrospinal fluid
Certain nerve pathways (called afferent neural pathways) induce vomiting when triggered by motion, ear infections or tumors, Ménière’s disease (a disease characterized by recurrent vertigo), odors, visual stimulation, pain, and bad tastes.
Still other nerve pathways (peripheral afferent neural pathways) induce vomiting in response to stomach irritants, distension of the intestines and bile ducts, abdominal inflammation, and myocardial infarction (heart attack).
The physical act of vomiting is controlled by multiple sites of the brain stem. When activated, these structures send signals to the throat, diaphragm, and abdominal muscles.
These signals result in the simultaneous contraction of these muscles, which brings the stomach contents up through the esophagus (the tube between the stomach and the throat) and out the mouth.
During vomiting, breathing is inhibited, except for short breaths between discharges. Bradycardia (decrease in the heart rate) and changes in blood pressure may occur during retching and vomiting.
Causes and symptoms
Vomiting can be caused by many different things. Vomiting that lasts only one or two days is usually caused by infection, a reaction to medication, a toxin, uremia (accumulation of protein breakdown products in the bloodstream), and diabetic ketoacidosis (accumulation of toxins resulting from uncontrolled diabetes).
Vomiting that lasts longer than one week can be caused by a long-term medical or psychiatric condition. Causes of vomiting include:
- Medications
. Drugs are the most common cause of vomiting, especially during the first days of use. Drugs can induce vomiting by stimulation of the area postrema or by direct stimulation of peripheral nerve pathways. Medications that commonly cause vomiting include cancer drugs, pain relievers (especially opioids), heart medications, diuretics, hormones, antibiotics, antiasthmatics, gastrointestinal drugs, and medications that act on the brain.
- Infections. Infections of the gastrointestinal system or whole body can cause vomiting. Gastrointestinal infections are more common in infants, toddlers, and young adults (20–29 years old) who usually get 1.2 infections each year. Infections that can cause vomiting include bacterial, viral, and parasitic gastrointestinal infections, severe acute respiratory syndrome (SARS), otitis media (ear infection), meningitis (infection of the membrane that surrounds the brain and spinal cord), and hepatitis (infection of the liver).
- Gastrointestinal and abdominal disorders. Disorders of the gastrointestinal system that can produce vomiting include blockage of the stomach or small intestine, motility disorders (muscles in the esophagus become discoordinated or weak, causing difficulty swallowing, regurgitation, and sometimes pain), indigestion, radiation therapy-induced changes, Crohn’s disease (chronic recurrent inflammation of the intestines), peptic ulcer, worm infestations, or inflammation of the appendix, gall bladder, or pancreas.
- Nervous system disorders. Cancers, infarction (an area of dead tissue caused by an obstruction in the artery supplying the area), bleeding (hemorrhage), birth defects, ear disorders, motion sickness, weightlessness, ear tumors, Ménière’s disease, unpleasant memories, psychogenic (caused by mental factors) issues, and bad tastes or smells can all cause vomiting.
- Hormones and physiological conditions. Hormonal and metabolic (physical and chemical processes of the body) conditions that can cause vomiting include: parathyroidism, diabetic ketoacidosis, hyperthyroidism (condition caused by excessive ingestion or production of thyroid hormone), Addison’s disease, uremia, and pregnancy. Pregnancy is the most common cause of vomiting associated with the hormonal system. Vomiting associated with pregnancy is often called morning sickness.
- Postoperation. Anesthesia and pain medications can cause nausea and vomiting, which are complications associated with 17–39% of surgeries.
- Cyclic vomiting syndrome (CVS). This rare disorder occurs in children usually beginning at age five years, although it also occurs in adults. It is characterized by, on average, eight attacks of vomiting lasting for 20 hours each year. Although the exact cause is unknown, there seems to be a relationship between cyclic vomiting and migraine headaches.
- Poisons. Arsenic and other heavy metals, weed killers and household cleaning agents, and many other substances may cause vomiting if inhaled or swallowed.
- Miscellaneous causes. Excessive alcohol consumption causes vomiting by acting both on the gastrointestinal tract and the brain.
Nausea is often associated with vomiting. Vomiting may be preceded by retching, in which the muscles contract as for vomiting but without the discharge of stomach contents.
The patient may hyperventilate (breathe rapidly and deeply) and salivate before vomiting begins. Patients should consult a physician immediately if there is blood in the vomitus (expelled stomach contents).
Other symptoms associated with vomiting depend upon the cause. Gastrointestinal infection would also cause fever, muscle pain, and diarrhea.
Patients with peptic ulcer, intestinal blockage, cholecystitis or pancreatitis (inflammation of the gall bladder or pancreas) would experience abdominal pain. Meningitis symptoms include neck stiffness, headache, vision changes, and changes in mental processes.
Diagnosis
Vomiting may be diagnosed by an internal medicine specialist or a gastroenterologist. A detailed medical history will be taken and will include specifics about the vomiting including frequency, a description of the vomitus, duration, how soon after meals vomiting occurs, and any other symptoms.
The history alone can help the physician to narrow down the cause to a few choices. The patient’s abdomen will be palpated (felt with the hands) to detect any abnormalities. Vital signs will be taken to identify any abnormalities in heart rate, blood pressure, or temperature.
Although the medical history and physical exam is usually sufficient to determine the cause of vomiting, certain laboratory tests may also be performed.
Blood tests may be performed to check for dehydration (decreased water), anemia (decreased number of red blood cells or iron-poor blood), and electrolyte (blood chemicals) imbalances, as well as specific tests to confirm the suspected diagnosis.
In some cases, more advanced testing may be required. These include x rays, endoscopy (a thin, wandlike camera used to visualize internal organs), magnetic resonance imaging (MRI), ultrasound (using sound waves to visualize internal organs), and computed tomography (CT) scanning. In addition, there are tests that measure stomach emptying and the pressure and motility of the stomach and intestine.
Treatment
Alternative treatments can be effective in treating vomiting, but not the underlying cause. A physician should be consulted if vomiting is recurrent and/or lasts for more than a few days.
Dietary changes
The best dietary approach is to eat foods that can be quickly cleared from the stomach. Foods that are high in fat are slow to digest and place the patient at risk for additional vomiting.
Ingestion of a low-fat, predominately liquid diet taken in frequent small meals can help relieve vomiting. Dry soda crackers are a good choice when nausea sets in. After vomiting, the patient should not eat for one hour, after which small servings of broth, bread, or flat soda may be taken.
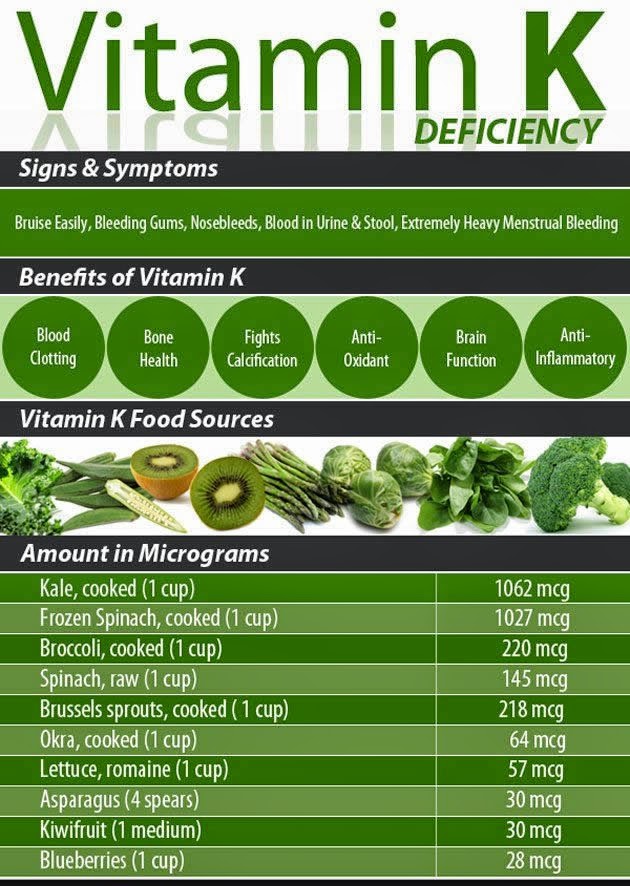
It is important to replenish the fluids lost by vomiting. Juice therapists recommend drinking a juice made from fresh ginger, apples, and carrots. Supplementation with vitamin B6 was found to reduce the symptoms of morning sickness in pregnant women.
Herbals
The herbs that are effective in relieving nausea and vomiting include:
- apple tree (Pyrus malus) bark tea
- bergamot (Monarda citriodora) tea
- black horehound (Ballota nigra) infusion
- codonopsis (Codonopsis pilosula) decoction
- galangal (Alpinia officinarum) infusion
- ginger (Zingiber officinale) infusion or crystallized
- lemongrass (Cymbogen citratus) oil or tea
- nutmeg (Myristica fragrans) capsules
- turmeric (Curcuma longa) infusion
Chinese medicine
Practitioners of traditional Chinese medicine use acupuncture, ear acupuncture, herbals, and patent medicines in the treatment of vomiting.
The following herbals may be made into soups, which are sipped frequently: Lu Gen
Placing a drop of Sheng Jiang (Rhizoma zingiberis recens) on the tongue can check vomiting. Patent medicines used to treat vomiting include: Huo Xiang Zheng Qi Wan (Agastache Pill to Rectify Qi),Yu Shu Dan (Jade Pivot Pill), Zuo Jin Wan (Left Metal Pill), and Bao He Wan
Homeopathy
Homeopathic remedies are chosen based upon the specific set of symptoms displayed by the patient. Ipecac is chosen for strong nausea and vomiting. Bismuth or Phosphorous is indicated when vomiting is caused primarily by liquids.
Nux vomica is recommended when vomiting is caused by emotional stress and for patients with heartburn, nausea, and retching. Tabacum is indicated for vomiting caused by motion. Veratrum album is indicated for the patient with nausea, vomiting, and diarrhea.
Arsenicum is recommended for the patient with violent vomiting, diarrhea, abdominal pain, exhaustion, restlessness, and thirst. Bryonia is recommended for gastroenteritis (inflammation of the lining of the gastrointestinal system).
Ayurveda
Ayurvedic practitioners believe that vomiting is caused by high pitta in the stomach. Remedies for vomiting are:
- yogurt containing cardamon and honey
- warm milk containing cardamon and nutmeg
- tea prepared from cumin seeds and nutmeg
- fresh pineapple juice (1 cup with a pinch of ginger and black pepper and 0.5 tsp sugar) three times during a day of fasting
- water containing 10 drops lime juice, 0.5 tsp sugar, and 0.25 tsp baking soda
- cardamon seeds (chewed)
- ginger juice and onion juice (1 tsp each)
- water containing rose petal powder (0.5 tsp), sandalwood powder (0.25 tsp), rock candy powder (0.5 tsp), and lime juice (10 drops)
Other treatments
Various other treatments for vomiting include:
- Aromatherapy. The essential oil of peppermint is a traditional cure for vomiting.
- Acupressure. The acupressure points P5 and P6 located on the inner forearms are effective in treating vomiting. A wristband (Sea-Band) has been proven to be effective in reducing nausea and vomiting.
- Acupuncture. A National Institutes of Health consensus panel found that acupuncture is an effective treatment for chemotherapy and postoperative vomiting. A few people, however, experience nausea as a side effect of acupuncture.
- Behavioral interventions. Behavioral therapies such as desensitization, distraction, imagery, relaxation, and self-hypnosis have been shown to be effective in treating chemotherapy-induced vomiting.
- Hydrotherapy. Stomach upsets may be treated by drinking a glass of water containing activated charcoal powder.
- Reflexology. The reflex points solar plexus, chest, lung, diaphragm, esophagus, liver, stomach, gallbladder and thyroid, and pituitary and adrenal gland on the feet may help treat vomiting.
- Transcutaneous electrical nerve stimulation (TENS, which is a treatment where a mild electrical current is passed through electrodes on the skin to stimulate nerves and block pain signals). TENS can be effective in reducing postoperative vomiting.
Allopathic treatment
Treatment of vomiting depends upon the cause and severity but may include dietary changes, medications, and surgery. Replacement of lost fluids is an important component of treatment.
Hospitalization may be required in some cases. Surgery may be needed to treat inflammatory conditions (such as cholecystitis) and physical abnormalities (such as blockage).
Medications used to treat vomiting are called antiemetics. Scopolamine, dimenhydrinate (Dramamine), and hyoscine are used to treat motion sickness; promethazine (Mepergan, Phenergan) is used to treat postoperative nausea; meclizine (Antivert, Bonine) is used to treat inner ear inflammation; and prochlorperazine (Compazine) is used for gastroenteritis, postoperative toxins, radiation, medications, and other causes of vomiting. Other medications that target the underlying cause of the vomiting may be used.
Newer drugs that have been developed to treat postoperative or postchemotherapy nausea and vomiting include ondansetron (Zofran) and granisetron (Kytril). Another treatment that has been found to lower the risk of nausea after surgery is intravenous administration of supplemental fluid before the operation.
Expected results
Most cases of vomiting resolve spontaneously. Complications of vomiting include dehydration, malnutrition, weight loss, and abnormalities of blood chemicals (including electrolytes, pH, and potassium). Vomiting by unconscious patients can lead to aspiration (inhalation of stomach contents), which can affect the lungs.
Prevention
Antiemetic drugs are effective at preventing vomiting. Some alternative treatments are effective at reducing nausea, which may prevent vomiting.