Tuberculosis
 |
| Tuberculosis |
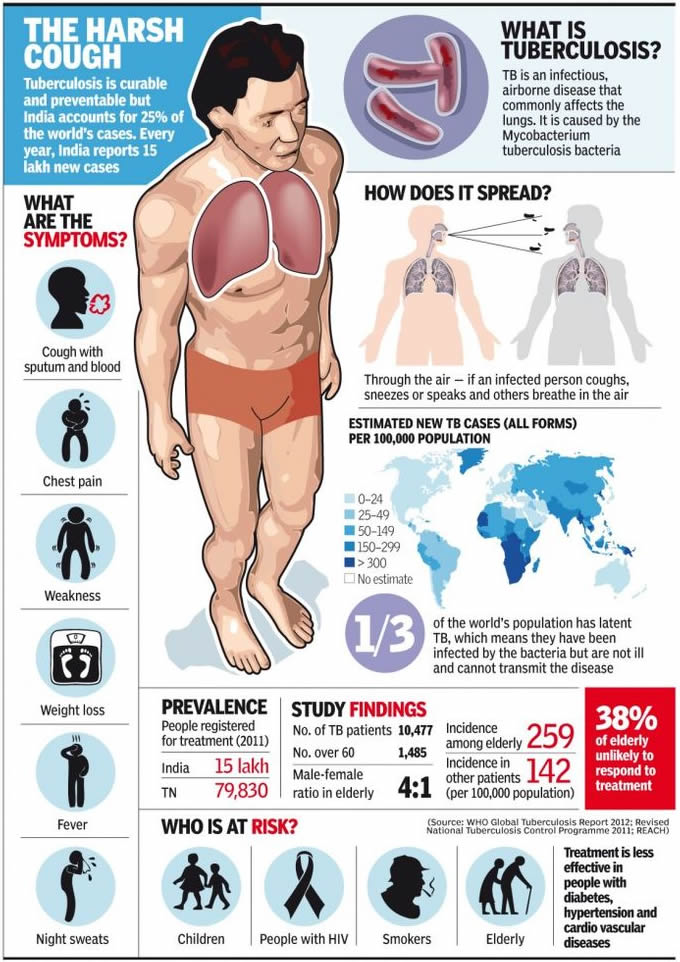
Tuberculosis (TB) is a contagious and potentially fatal disease that can affect almost any part of the body but manifests mainly as an infection of the lungs. It is caused by a bacterial microorganism, the tubercle bacillus or Mycobacterium tuberculosis. TB infection can either be acute and short-lived or chronic and long-term.
Although TB can be prevented, treated, and cured with proper treatment and medications, scientists have never been able to eliminate it entirely. The organism that causes tuberculosis, popularly known as consumption, was discovered in 1882.
Because antibiotics were unknown, the only means of controlling the spread of infection was to isolate patients in private sanatoria or hospitals limited to patients with TB—a practice that continues to this day in many countries. TB spread very quickly and was a leading cause of death in Europe.
  |
At the turn of the twentieth century more than 80% of the people in the United States were infected before age 20, and tuberculosis was the single most common cause of death. Streptomycin was developed in the early 1940s and was the first antibiotic effective against the disease.
The number of cases declined until the mid- to late-1980s, when overcrowding, homelessness, immigration, decline in public health inspections, decline in funding, and the AIDS epidemic caused a slight resurgence of the disease. The increase in TB in the United States peaked in 1992, and new cases reported in the United States continue to decrease as of 2004.
Yet the number of cases in foreign-born individuals is rising, and the number of deaths from TB has been rising, making TB a leading cause of death from infection throughout the world. It is estimated that in the next 10 years 90 million new cases of TB will be reported, with the result of 30 million deaths, or about 3 million deaths per year.
Several demographic groups are at a higher risk of contracting tuberculosis. Tuberculosis is more common in elderly persons. More than one-fourth of the nearly 23,000 cases of TB in the United States in 1995 were reported in people above age 65. TB also is more common in populations where people live under conditions that promote infection, such as homelessness and injection drug use.
In the late 1990s, two-thirds of all cases of TB in the United States affected African Americans, Hispanics, Asians, and persons from the Pacific Islands. Finally, the high risk of TB includes people who have a depressed immune system.
High-risk groups include alcoholics, people suffering from malnutrition, diabetics, and AIDS patients — and those infected by human immunodeficiency virus (HIV) — who have not yet developed clinical signs of AIDS. TB is the number one killer of women of childbearing age worldwide. In poor countries, women with TB often don’t know they have the disease until symptoms become severe.
As of late 2002, TB is a major health dilema in certain immigrant communities, such as the Vietnamese in southern California. One team of public health experts in North Carolina maintains that treatment for tuberculosis is the most pressing healthcare need of recent immigrants to the United States.
In some cases, the vulnerability of immigrants to tuberculosis is increased by occupational exposure, as a recent outbreak of TB among Mexican poultry farm workers in Delaware indicates. Other public health experts are recommending tuberculosis screening at the primary care level for all new immigrants and refugees.
 |
| Tuberculosis infographic |
Causes and symptoms
Transmission
Tuberculosis spreads by droplet infection, in which a person breathes in the bacilli released into the air when a TB patient exhales, coughs, or sneezes.
However, TB is not considered highly contagious compared to other infectious diseases. Only about one in three people who have close contact with a TB patient, and fewer than 15% of more remote contacts, are likely to become infected.
Unlike many other infections, TB is not passed on by contact with a patient’s clothing, bed linens, or dishes and cooking utensils. Yet if a woman is pregnant, her fetus may contract TB through blood or by inhaling or swallowing the bacilli present in the amniotic fluid.
Once inhaled, water in the droplets evaporates and the tubercle bacilli may reach the small breathing sacs in the lungs (the alveoli), then spread through the lymph vessels to nearby lymph nodes. Sometimes the bacilli move through blood vessels to distant organs.
At this point they may either remain alive but inactive (quiescent), or they may cause active disease. The likelihood of acquiring the disease increases with the concentration of bacilli in the air, and the seriousness of the disease is determined by the number of bacteria with which a patient is infected.
Ninety percent of patients who harbor M. tuberculosis do not develop symptoms or physical evidence of the disease, and their x rays remain negative. They are not contagious; however, these individuals may get sick at a later date and then pass on TB to others.
Though it is impossible to predict whether a person’s disease will become active, researchers surmise that more than 90% of cases of active tuberculosis come from this pool of people. An estimated 5% of infected persons get sick within 12-24 months of being infected.
Another 5% heal initially but, after years or decades, develop active tuberculosis. This form of the disease is called reactivation TB, or post-primary disease. On rare occasions a previously infected person gets sick again after a second exposure to the tubercle bacillus.
Pulmonary tuberculosis
Pulmonary tuberculosis is TB that affects the lungs, and represents about 85% of new cases diagnosed. It usually presents with a cough, which may or may not produce sputum. In time, more sputum is produced that is streaked with blood.
The cough may be present for weeks or months and may be accompanied by chest pain and shortness of breath. Persons with pulmonary TB often run a low-grade fever and suffer from night-sweats. The patient often loses interest in food and may lose weight.
If the infection allows air to escape from the lungs into the chest cavity (pneumothorax) or if fluid collects in the pleural space (pleural effusion), the patient may have difficulty breathing. The TB bacilli may travel from the lungs to lymph nodes in the sides and back of the neck. Infection in these areas can break through the skin and discharge pus.
Extrapulmonary tuberculosis
Although the lungs are the major site of damage caused by tuberculosis, many other organs and tissues in the body may be affected. About 15% of newly diagnosed cases of TB are extrapulmonary, with a higher proportion of these being HIV-infected persons. The usual progression of the disease is to begin in the lungs and spread to locations outside the lungs (extrapulmonary sites).
In some cases, however, the first sign of disease appears outside the lungs. The many tissues or organs that tuberculosis may affect include:
- Bones. TB is particularly likely to attack the spine and the ends of the long bones.
- Kidneys. Along with the bones, the kidneys are probably the most common site of extrapulmonary TB. There may, however, be few symptoms even though part of a kidney is destroyed.
- Female reproductive organs. The ovaries in women may be infected; TB can spread from them to the peritoneum, which is the membrane lining the abdominal cavity.
- Abdominal cavity. Tuberculous peritonitis may cause pain ranging from the mild discomfort of stomach cramps to intense pain that may mimic the symptoms of appendicitis.
- Joints. Tubercular infection of joints causes a form of arthritis that most often affects the hips and knees.
- Meninges. The meninges are tissues that cover the brain and the spinal cord. Infection of the meninges by the TB bacillus causes tuberculous meningitis, a condition that is most common in young children and the elderly. It is extremely dangerous. Patients develop headaches, become drowsy, and eventually comatose. Permanent brain damage can result without prompt treatment.
- Skin, intestines, adrenal glands, and blood vessels. All these parts of the body can be infected by M. tuberculosis. Infection of the wall of the body’s main artery (the aorta), can cause it to rupture with catastrophic results. Tuberculous pericarditis occurs when the membrane surrounding the heart (the pericardium) is infected and fills up with fluid that interferes with the heart’s ability to pump blood.
- Miliary tuberculosis. Miliary TB is a life-threatening condition that occurs when large numbers of tubercle bacilli spread throughout the body. Huge numbers of tiny tubercular lesions develop that cause marked weakness and weight loss, severe anemia, and gradual wasting of the body.
Diagnosis
TB is diagnosed through laboratory test results. The standard test for tuberculosis infection, the tuberculin skin test, detects the presence of infection, not of active TB. Skin testing has been done for more than 100 years. In this process, tuberculin is an extract prepared from cultures of M. tuberculosis.
It contains substances belonging to the bacillus (antigens) to which an infected person has been sensitized. When tuberculin is injected into the skin of an infected person, the area around the injection becomes hard, swollen, and red within one to three days.
Today skin tests utilize a substance called purified protein derivative (PPD) that has a standard chemical composition and is therefore a good measure of the presence of tubercular infection.
The PPD test, also called the Mantoux test, is not always 100% accurate; it can produce false positive as well as false negative results. The test may indicate that some people who have a skin reaction are not infected (false positive) and that some who do not react are in fact infected (false negative).
The PPD test is, however, useful as a screener and can be used on people who have had a suspicious chest x ray, on those who have had close contact with a TB patient, and persons who come from a country where TB is common.
Because of the multiple and varied symptoms of TB, diagnosis on the basis of external symptoms is not always possible. TB is often discovered by an aneh chest x ray or other test result rather than by a claim of physical discomfort by the patient. After an irregular x ray, a PPD test is always done to show whether the patient has been infected.
To verify the test results, the physician obtains a sample of sputum or a tissue sample (biopsy) for culture. In cases where other areas of the body might be infected, such as the kidney or the brain, body fluids other than sputum (urine or spinal fluid, for example) can be used for culture.
One important new advance in the diagnosis of TB is the use of molecular techniques to speed the diagnostic process as well as improve its accuracy. As of late 2002, four molecular techniques are increasingly used in laboratories around the world.
They include polymerase chain reaction to detect mycobacterial DNA in patient specimens; nucleic acid probes to identify mycobacteria in culture; restriction fragment length polymorphism analysis to compare different strains of TB for epidemiological studies; and genetic-based susceptibility testing to identify drug-resistant strains of mycobacteria.
Treatment
Because of the nature of tuberculosis, the disease should never be treated by alternative methods alone. Alternative treatments can help support healing, but treatment of TB must include drugs and will require the care of a physician. Any alternative treatments should be discussed with a medical practitioner before they are applied.
Supportive treatments include:
- Diet. Nutritionists recommend a whole food diet including raw foods, fluids, and particularly pears and pear products (pear juice, pear sauce), since pears may help heal the lungs. Other helpful foods include fenugreek, alfalfa sprouts, garlic, pomegranate, and yogurt or kefir. Four tablespoons of pureed steamed asparagus at breakfast and dinner taken for a few months may also be helpful.
- Nutritional therapy. Nutritionists may recommend one or many of the following vitamins and minerals: vitamin A at 300,000 IU for the first three days, 200,000 IU for the next two days, then 50,000 IU for several weeks; beta-carotene at 25,000-50,000 IU; vitamin E at up to 1,000 IU daily unless the patient is a premenopausal woman with premenstrual symptoms; lipotrophic formula (one daily); deglycerolized licorice; citrus seed extract; vitamin C; lung glandular; essential fatty acids; vitamin B complex; multiminerals; and zinc.
- Herb therapy may use the tinctures of echinacea, elecampane, and mullein taken three times per day, along with three garlic capsules three times per day.
- Hydrotherapy may be used up to five times weekly. Dr. Benedict Lust, the founder of naturopathy, supposedly cured himself of tuberculosis by using hydrotherapy.
- Juice therapy. Raw potato juice, may be taken three times daily with equal parts of carrot juice plus one teaspoon of olive or almond oil, one teaspoon of honey, beaten until it foams. Before using the potato juice, starch should be allowed to settle from the juice.
- Topical treatment may use eucalyptus oil packs, grape packs or grain alcohol packs.
Professional practitioners may also treat tuberculosis using cell therapy, magnetic field therapy, or traditional Chinese medicine. Fasting may be undertaken, but only with a doctor’s supervision.
Allopathic treatment
Drug therapy
Five drugs are most commonly used today to treat tuberculosis: isoniazid (INH), rifampin, pyrazinamide, streptomycin, and ethambutol. Of the five medications, INH is the most frequently used drug for both treatment and prevention. The first three drugs may be given in the same capsule to minimize and treat active TB the number of pills in the dosage.
As of 1998, many patients are given INH and rifampin together for six months, with pyrazinamide added for the first two months. Hospitalization is rarely necessary because many patients are no longer infectious after about two weeks of combination treatment. A physician must monitor side effects and conduct monthly sputum tests.
In 2002, the Centers for Disease Control (CDC) worked with medical organizations to release new guidelines that better individualize the drug regimens received by TB patients depending on their disease symptoms and severity. Many can now receive once-weekly doses of rifapentine in the continuation phase of treatment.
The first large scale trial of a new agent to treat TB began in 2002. The promising new drug, called moxifloxacin, may mean a shorter treatment course for TB sufferers in the near future.
It will also be tested in combination with rifapentine, and researchers believe that using the drugs together will mean a less frequent dosing schedule for patients.
Drug resistance has become a dilema in treating TB. When patients do not take medication properly or for long enough periods of time, the TB organisms may become drug resistant. This makes the patient vulnerable to further infection and allows the TB organism to develop resistance.
Surgery
Surgical treatment of TB may be used if medications are ineffective. There are three surgical treatments for pulmonary TB: pneumothorax, in which air is introduced into the chest to collapse the lung; thoracoplasty, in which one or more ribs are removed; and removal of a diseased lung, in whole or in part. It is possible for patients to survive with one healthy lung.
Expected results
The prognosis for recovery from TB is good for most patients, if the disease is diagnosed early and given prompt treatment with appropriate medications on a long-term regimen.
According to a 2002 Johns Hopkins study, most patients in the United States who die of TB are older—average age 62— and suffer from such underlying diseases as diabetes and kidney failure.
Modern surgical methods are usually effective when necessary. Miliary tuberculosis is still fatal in many cases but is rarely seen today in developed countries.
Even in cases in which the bacillus proves resistant to all of the commonly used medications, other seldom-used drugs may be tried because the tubercle bacilli have not yet developed resistance to them.
Prevention
Vaccination is widely used as a prevention measure for TB. A vaccine called BCG (Bacillus Calmette-Guérin, named after its French developers) is made from a weakened mycobacterium that infects cattle.
Vaccination with BCG does not prevent infection, but it does strengthen the immune system of first-time TB patients. As a result, serious complications are less likely to develop. BCG is used more widely in developing countries than in the United States.
Though the vaccine has been proven beneficial and fairly safe, its use is still controversial. It is not clear whether the vaccine’s effectiveness depends on the population in which it is used or on variations in its formulation. Recently, efforts have been focused on developing a new vaccine.
Generally, prevention focuses on the prevention of transmission, skin-testing high-risk persons and providing preventive drug therapy to people at risk.
Measures such as avoidance of overcrowded and unsanitary conditions are necessary aspects of prevention. Hospital emergency rooms and similar locations can be treated with ultraviolet light, which has an antibacterial effect.
INH is also given to prevent TB, and decreases the incidence of TB by about 60% over the life of the patient. INH is effective when taken daily for 6 to 12 months by people in high-risk categories who are under 35 years of age.
About 1% of patients in preventive treatment develop toxicity. Because INH carries the risk of side effects (liver inflammation, nerve damage, changes in mood and behavior), it is important for its use to be monitored and to give it only to persons at special risk.
Unfortunately, failure of TB patients to complete the full course of their drugs adds to TB incidence and encourages development of drug-resistant strains of the disease.
As scientists try to develop drugs that require shorter courses, physicians must work with patients to encourage compliance with their treatments. Even if symptoms go away, patients often have to continue their drug treatment for six months to be sure to stop the spread of their TB infection to others.