Warts, also called verrucae, are small benign growths usually caused by a viral infection of the skin or mucous
membrane. The virus infects the surface layer of skin. The viruses that cause warts are members of the human papilloma virus (HPV) family, of which there are many different strains.
Warts are not cancerous but some strains of HPV, usually not associated with warts, have been linked with cancer formation. Warts are contagious from
person to person and from one area of the body to another on the same person.
Particularly common among children, young adults, and women, warts are a masalah for 7–10% of the
population. There are close to 60 types of HPV that cause warts, each preferring a specific skin location.
For instance, some types of HPV cause warts to grow on the skin, others cause them to grow inside the mouth, while still others cause them to grow on the genital and rectal areas.
However, most can be active anywhere on the body. The virus enters through the skin and produces new warts after an incubation period of one to eight months. Warts are usually skin colored and feel rough to the touch, but they also can be dark, flat, and smooth.
Warts are passed from person to person, directly and indirectly. Some people are continually susceptible to warts, while others are more resistant to HPV and seldom get them.
The virus takes hold more readily when the skin has been damaged in some way, which may explain why children who bite their nails tend to have warts located on their fingers. People who take a medication to suppress their immune system or are on long-term steroid use are also prone to a wart virus infection. The same is true for patients with AIDS.
The main categories of warts are
common warts (face and hands), plantar warts (feet), and venereal warts. Hand warts (verruca vulgaris) can grow anywhere on the hands, but usually occur where skin has been damaged in some way (e.g. picking or nail biting). This is a rough horny lesion varying in size from 1 mm–2cm in diameter.
Foot warts (verruca plantaris) known as plantar warts, are the most painful type of wart, due to the pressure exerted on them. They are most common in children and young adults, since they are often contracted in locker rooms and swimming pool areas.
If left untreated, they can grow to an inch or more in circumference and spread into clusters. Those suffering from diabetes are more likely to suffer from plantar warts, and may also suffer complications due to the reduced potential for their bodies to heal themselves.
Flat warts tend to grow in great numbers and are smaller and smoother than other warts. They can erupt anywhere, appearing more frequently on the legs of women, the neck and dorsum of the hands, the faces of children, and on the areas of the face that are shaved by young adult males.
Genital warts, also called condylomata acuminata, moist warts, fig warts, or venereal warts, are one of the most common sexually transmitted diseases (STDs). Genital warts are more contagious than other types of warts.
Approximately one million new cases of genital warts are diagnosed in the United States every year. It is estimated that two-thirds of persons coming into contact with genital warts will develop symptoms within three months.
Genital warts tend to be small flat bumps or they may be thin and pointed in shape. They are usually soft, moist, pink to red in color, occurring as a single lesion or in clusters that resemble a cauliflower, and not scaly like other warts. In women, genital warts appear on the external genitalia, within the vagina, on the cervix, and around the anus or within the rectum.
In men, genital warts usually appear on the tip of the penis but may also be found on the scrotum or around the anus. Genital warts can also develop in the mouth of a person who has had oral
sexual contact with an infected person. They may also appear, less often, between the toes.
Filiform wart is a long, horny, finger-like projection that is usually found in multiples. Seen most commonly in adult males, they occur in the bearded area of the face or on the eyelids and neck.
Causes and symptoms Since warts are caused by a virus, they can only be caught by contact with a source of infection. This can be direct physical contact, or secondary contact with the shed skin of a wart (through a floor or a towel for example). As the incubation period for warts is quite long, it is often difficult to pinpoint sources of infection.
Individuals whose immune systems are deficient most often contract warts. AIDS patients commonly suffer from warts, and it is not uncommon for warts to appear at the site of a syok (burns, cuts or abrasions.)
Diagnosis Common warts are rough, irregular, skin colored or brownish. Warts that are brownish in color, or that do not respond to treatment, should be checked by a physician to exclude the possibility that they may be malignant growths.
Treatment Warts may need no treatment at all, since a large proportion of them (67% over a two-year period) disappear spontaneously. This is particularly so in the case of flat warts.
However, a wart that appears unusual in any way should be checked by a physician, as a small proportion can become malignant. Generally, the main criterion for treatment of warts is a cosmetic one, if it is found to be embarrassing by the sufferer, or unpleasant to others.
Acupuncture The aim with acupuncture will be to raise the general well-being of the patient, improve the functioning of the immune system, and free blockages of “chi” or life force. Warts and other health problems will be less likely to occur as general health and resistance are improved.
Aromatherapy Since warts are caused by viral infections, the aim of an aromatherapy treatment would be to kill the virus with the application of an appropriate essential oil. There are many oils that have antiviral properties, so the therapist will also endeavor to choose oils that are appropriate for the patient.
Onion and garlic oils both have powerful antiviral properties, but perhaps tea tree oil, which also possesses remarkable anti-viral properties, might be more acceptable as far as smell is concerned.
Colloidal silver The use of colloidal silver against viruses of all kinds has proved very successful. It should be topically applied to the wart, but can be taken internally to promote functioning of the immune system, and thus prevent warts from occurring.
Herbal medicine Herbal remedies for genital warts and other STDs have attracted considerable recent attention because of the epidemic spread of these diseases in developing countries where most people cannot afford allopathic treatments.
One traditional herbal remedy from Colombia that is being studied is extracts of plants belonging to the Euphorbia family. These compounds have been used to treat ulcers, tumors, and warts for generations, and some of them appear to be effective in treating genital warts.
Before applying any herbal cure to a wart, as much of the wart as possible should be removed, in order to give the cure a head start.
Apple juice: Apply the juice of a sour apple. Action is due to the magnesium in the juice.
Banana skin: First the wart should be rubbed with an abrader, and a fresh banana skin (immediately after opening) should be applied and left overnight.
Cabbage: Apply fresh juice from a white cabbage.
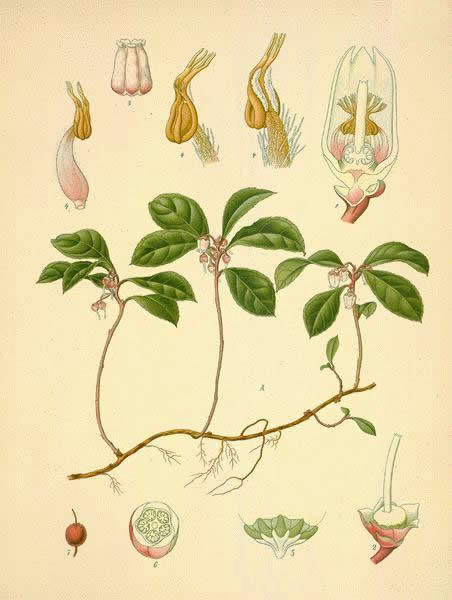
Chickweed: Apply the juice to the wart.
Dandelion: The juice of the dandelion is a very old English cure for warts.
Garlic: Rub a raw clove on the wart every night until it disappears.
Green figs: The white milk from a green fig is excellent at removing warts.
House leek: This is a plant commonly found in rock gardens. It has thick fleshy leaves and its juice is rich in supermalate of calcium, which will destroy warts.
Pineapple: Cotton wool should be soaked in the fresh juice of a pineapple. The enzymes of the pineapple will dissolve the wart.
Rubber plant: If the stem of a leaf from a rubber plant is broken, white liquid will ooze out. If this is applied to the wart over a period of two to three days, the wart should disappear.
Naturopathy Naturopathy, in common with many alternative therapies, works on the principle that given the right circumstances, such as pure air, pure water, and first class nutrition, the body will heal itself and become extremely resistant to illness. Naturopaths believe that such symptoms as warts are the result of toxins in the body, and an immune system that is not running efficiently.
They may prescribe treatments such as colonic irrigation, alongside a aktivitas of healthy eating to raise the general level of health. A naturopath may suggest a paste made with vitamin C, applied to the wart daily for a period of a few weeks.
Visualization This method, also known as creative imagery, has skeptically been described as “willing yourself well,” but practically it has been found to be very effective for a
range of conditions, both physical and emotional.
The patient is required to sit in a relaxed state, breathing evenly, and visualize the self in the condition he or she would like to be. In this case, perhaps he or she visualizes the body overcoming the warts and absorbing them, leaving behind healthy skin. This method has been found particularly suitable for children, as it has no side effects and therapists claim it has a good success rate.
Folk remedies There are many remedies for warts that have been handed down from generation to generation all over the world. The following remedies have excellent track records.
Thread: a length of thread should be tied around the wart, and tightened every day until the wart drops off.
Human saliva: the sufferer applies his or her saliva to the wart first thing every morning.
Allopathic treatment Warts may be self-treated by a number of allopathic remedies, but care should be taken as they are fairly strong chemicals (usually salicylic acid).
Those suffering from diabetes, heart disease or circulation problems, or any degree of peripheral neuropathy, should not attempt to treat themselves with any of these preparations, because of the risk of damage to tissue, and because of their increased susceptibility to infection.
In addition, the face and mucous membranes may scar, so it may be preferable to seek professional advice.
A physician may use cautery (use of heat) or cryosurgery (use of extreme cold, usually in the form of liquid nitrogen) to remove warts. These are processes that require precision, and therefore are highly skilled procedures.
Another drawback is that they can be painful. Increasingly, laser treatments are also being used to treat warts, whereby the laser beam vaporizes the wart tissue. Pulsed laser treatments appear to be particularly effective in treating warts in the anogenital region of children.
A newer allopathic medication that shows promise in the treatment of resistant viral facial warts is diphencyprone (DPC), a drug that was developed to treat a type of hair loss known as alopecia areata. DPC has shown effectiveness in removing facial warts that were resistant to both cryosurgery and other topical drugs.
Expected results Allopathic methods for the treatment of warts are generally successful, but they carry more risk of scarring than natural methods.
More than one alternative method may have to be tried before success is achieved, but they carry the added bonus of adding to the well-being of the patient, and not harming the body. Allopathic treatments involve the use of strong chemicals, which carry risks and are not compatible with body chemistry.
Usually, warts either disappear spontaneously or are treated successfully with no scarring or lasting effects. However, occasionally, what appears to be a wart is the beginning of a type of cancer, so those that are resistant to treatment should be seen by a physician.
Recurrent genital warts are a serious personal and public health concern. Even though genital warts may be removed, the virus itself continues to live. Certain types of HPV can cause tissue changes in the cervix of women with recurrent infection that may lead to cervical cancer.
The general recommendation for women who have a history of genital warts is to see their doctors every six months for Pap smears to monitor any changes that may occur.
Prevention To avoid foot warts, footwear should always be worn in public places and feet should be kept clean and dry. In general, warts should not be picked, to avoid cross infection, and any patch of damaged skin should be protected. Every effort should be made to keep the immune system in peak working condition.
Genital warts can be prevented by using condoms and avoiding unprotected sexual contact. Barrier protection will not, however, prevent the spread of wart-causing HPV to such uncovered areas as the pubis and upper thighs.
Although vaccines to prevent the spread of human papilloma virus are under investigation as of 2002, they will not be available for general use for at least several years.